How BHRT Can Help Patients Ease the Symptoms of Aging

Did you know that hormone replacement therapy can help reduce some of the symptoms of aging?
Everyone knows that we can’t stop the aging process and its associated physiological symptoms. Still, it’s only natural that patients become confused and distressed as they experience the sometimes dramatic health changes which arrive in mid-life.
Bioidentical hormone replacement therapy (BHRT) can help to ease their suffering and give them a new lease on life.
Hormones: A Delicate Balance
Both men and women experience a drop in hormone levels around mid-life. Culture, diet, and other lifestyle factors can affect the way hormones are produced in the body, as can surgery, injury, and trauma.
Women especially are looking for alternatives to conventional HRT to help with symptoms related to menopause and perimenopause.
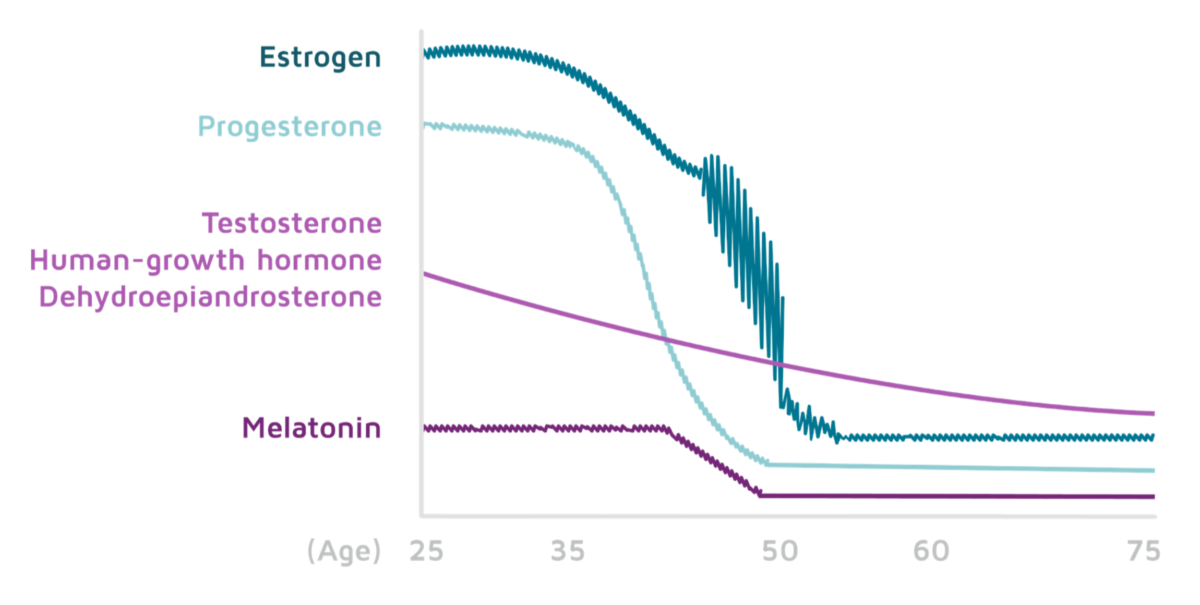
Gaining a clear understanding of how mid-life hormone fluctuations influence symptoms of aging is imperative to the proper administration of BHRT. And knowing how a patient’s hormone levels change over time is essential.
Although age is the primary reason that patients will seek BHRT, physicians should also be aware of reasons besides menopause/andropause which can cause hormone changes.
Progesterone Decline in Mid-Life
Progesterone which in women naturally start to drops around age 35, is part of at least 300 body functions and symptoms, including those related to:
- The central nervous symptom
- Mood
- Inflammation
- Cell reproduction
- Adrenal hormones
- Cognition
Since the hormone is so prevalent, changes in progesterone levels can affect women on a physical, gynecological, and emotional level.
Besides menopause/perimenopause, progesterone may drop due to oophorectomy, nutrient deficiencies, diet and microbiome, and high cortisol levels due to stress.
The range of symptoms possibly associated with progesterone deficiency is vast, so it can be difficult to determine whether a deficiency is the root cause.
Still, if patients complain of mood swings, PMS, heavy or irregular cycles, hair loss, and even allergies, you may want to consider testing for progesterone deficiency and compare against estrogen levels to determine treatment for symptoms of aging.
Read more: Four Common Types of Hormone Imbalance
Estrogen Imbalances
Estrogen normally begins to decline later than progesterone and can be expected to drop around age 50, leading to less frequent menstruation and menopause.
But women often experience serious symptoms during this time because estrogen levels can be erratic, changing from month-to-month and wreaking havoc on almost all bodily symptoms. It’s here we typically see significant menopause-related symptoms like:
- Hot flashes
- Depression
- Brain “fog”
- Vaginal dryness
- Insomnia
- Dry skin and hair
- Weight gain
- Joint and bone inflammation
- Aches and pains
These symptoms can trigger others if not kept in check. To add to this, progesterone drops make the estrogen drop worse since progesterone influences the sensitivity of estrogen receptors.
So getting a hold of monthly changes in estrogen levels is crucial for health care providers who want to offer BHRT to minimize and even combat symptoms of aging.
The balance of the two should always be considered and monitored when treating for menopause and monitored also in light of cortisol and catecholamine levels.
Andropause and Testosterone Decline
Although women tend to be much more sensitive to mid-life hormone changes on average, men are not immune to hormone-influenced symptoms of aging.
Testosterone typically drops into mid-age, and around age 40 it is about half of what it was in their 20s, with the exception of external factors such as injury or surgery.
Men also can experience lower libido, erectile problems, mood changes, and lower bone and muscle mass.
Men’s testosterone levels are particularly tied to the adrenal glands, so depression can both be tied in with testosterone levels.
Effectively Prescribing BHRT for Hormone Imbalances
Unfortunately, a basic FSH test won’t result in the detailed information needed to actually see the nuances involved in hormone imbalances.
But capillary blood spot serum, saliva, and dried urine tests can help to get a better understanding of endogenous hormone levels.
Comprehensive lab testing typically also suggests optimal ranges. That being said, lab values that fall in “normal” ranges do not necessarily reflect “optimal” levels for a person.
But given that BHRT has the potential to not only reduce some basic symptoms of aging but possibly even some more serious health problems like heart disease and arthritis, it’s important that people in high-risk categories are offered testing which goes beyond what would be offered for standardized (conventional) HRT.
It is the unique testing processes and the capacity for BHRT to offer individualized treatment that can make it so effective.
Start Prescribing BHRT Today
What will you do for your patients if they come to you with symptoms of aging but you are not able to offer them complete treatment?
Given the increasing demand for this type of therapy, physicians and other health providers should learn how to prescribe bioidentical hormone replacement therapy as a potentially safer and effective option for wellness management through mid-life hormone decline.
Considering BHRT as an addition to your practice? There couldn’t be a better time. Click here to schedule a free strategy call.
Enjoyed this article? Here are three more to help you:
BHRT is a Movement – It’s Not Going Away
The Benefits of Opening a Bioidentical Hormone Practice
Pros and Cons of Different Dosing Forms of Bioidentical Hormones
Get the quick read ebook,
Getting Started with BHRT -
Key Insights to Prescribing and Implementing BHRT.
CME's - Earn while you learn.